Specialized gastric interventions customized for your condition, providing effective treatment for digestive disorders, pain relief, and improved quality of life.
Dr. Nguyen specializes in a range of advanced stomach procedures tailored to address various digestive disorders and conditions. Each surgical approach is designed to effectively treat the underlying problem, alleviate symptoms, and restore proper gastric function while using the most appropriate techniques for your specific diagnosis.
Explore our stomach procedure options below to discover which approach might be most suitable for your specific condition and personal digestive health needs.
.webp)
This precise surgical procedure removes part or all of the stomach to address serious conditions such as cancer, bleeding, perforation, or certain severe digestive disorders unresponsive to other treatments.
What happens during surgery?
Using either minimally invasive techniques or an open approach depending on your specific condition, your surgeon carefully removes the affected portion of the stomach. The remaining sections are reconnected to preserve digestive continuity whenever possible. For total gastrectomy, the esophagus is connected directly to the small intestine. The entire procedure typically takes 2-4 hours under general anesthesia.
Benefits:
Effective treatment or potential cure for gastric cancer and precancerous conditions
Resolution of uncontrollable bleeding or perforation issues
Relief from symptoms of certain advanced stomach disorders
Minimally invasive options available for appropriate candidates
Preservation of digestive function through careful reconstruction
Long-term solution for conditions unresponsive to medication or other therapies
Gastrectomy provides a definitive intervention for serious gastric conditions, effectively addressing the underlying problem while maintaining the best possible digestive function through meticulous surgical technique and reconstruction.
This specialized procedure addresses complicated peptic ulcers by modifying stomach anatomy and nerve supply to reduce acid production and improve stomach emptying, treating ulcers that haven't responded to medication.
What happens during surgery?
Using minimally invasive techniques when possible, your surgeon performs one or both components: pyloroplasty widens the stomach outlet (pylorus) to improve emptying, while vagotomy involves cutting specific branches of the vagus nerve to reduce stomach acid production. These precise modifications help prevent ulcer recurrence and complications. The entire procedure typically takes 1-3 hours under general anesthesia.
Benefits:
Effective treatment for ulcers resistant to medical therapy
Prevention of serious ulcer complications like perforation and bleeding
Reduced stomach acid production to promote healing
Improved stomach emptying and reduced pressure on the digestive tract
Relief from chronic pain and digestive discomfort
Decreased likelihood of ulcer recurrence
Ulcer repair surgery offers a durable solution for patients with complicated or treatment-resistant peptic ulcers, addressing both symptoms and underlying causes to provide long-term relief and prevent potentially life-threatening complications.

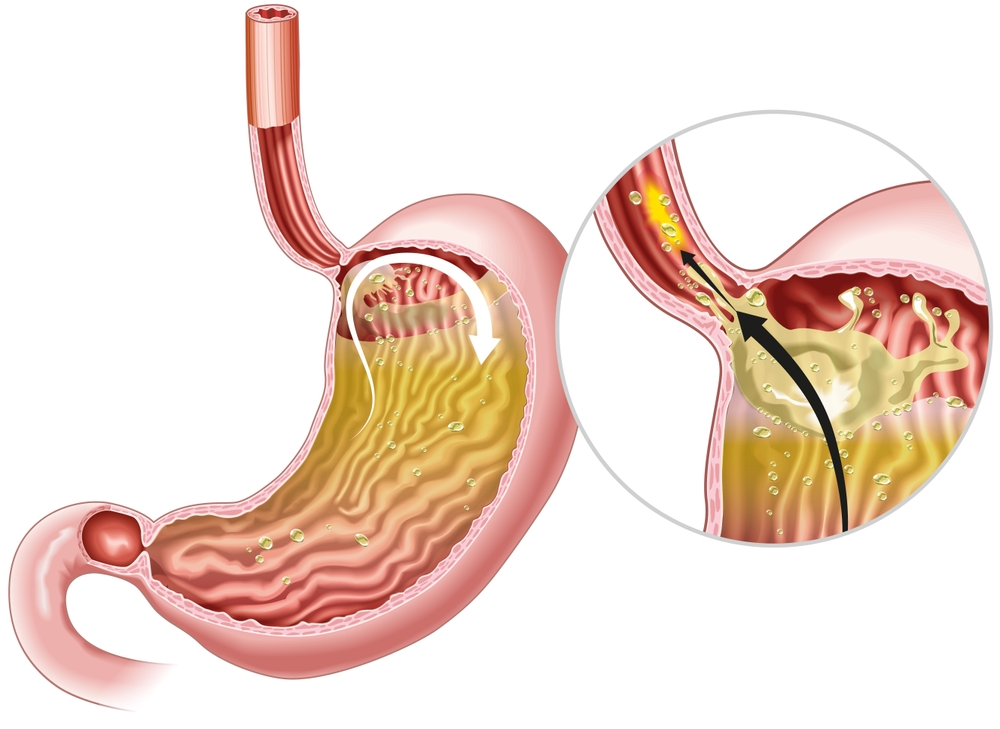
This precise anti-reflux procedure wraps the upper portion of the stomach around the lower esophagus, creating a stronger barrier that prevents stomach acid from flowing upward and eliminates chronic heartburn and GERD symptoms.
What happens during surgery?
Using minimally invasive techniques whenever possible, your surgeon accesses the junction where the esophagus meets the stomach. The upper part of the stomach (fundus) is carefully wrapped around the lower esophagus and secured with stitches, creating a one-way valve effect that allows food to pass down while preventing acid from refluxing upward. The entire procedure typically takes 1-2 hours under general anesthesia.
Benefits:
Significant reduction or elimination of acid reflux symptoms
Decreased dependence on daily acid-reducing medications
Protection of the esophagus from ongoing acid damage
Reduced risk of Barrett's esophagus and esophageal cancer
Improvement in related symptoms like chronic cough and asthma
Long-lasting results for most patients (typically 10+ years)
Nissen fundoplication offers a durable solution for severe GERD that doesn't respond adequately to medication, allowing patients to enjoy meals without painful reflux while protecting long-term esophageal health and improving overall quality of life.
This corrective procedure addresses the protrusion of the stomach through the diaphragm into the chest cavity, repositioning the stomach and reinforcing the weakened diaphragmatic opening to alleviate symptoms.
What happens during surgery?
Using minimally invasive techniques in most cases, your surgeon carefully returns the portion of stomach that has moved into the chest cavity back to its proper position below the diaphragm. The enlarged opening in the diaphragm is narrowed with sutures, and the area is often reinforced. A partial fundoplication may be performed simultaneously to prevent reflux. The entire procedure typically takes 1-2 hours under general anesthesia.
Benefits:
Significant reduction in heartburn, regurgitation, and chest pain
Relief from difficulty swallowing and the feeling of food getting stuck
Prevention of serious complications like strangulation
Reduced risk of aspiration pneumonia and respiratory issues
Minimized post-operative discomfort with laparoscopic approaches
Long-lasting correction of the anatomical defect
Hiatal hernia repair offers effective treatment for persistent symptoms and structural abnormalities, allowing patients to eat comfortably and sleep without the discomfort of stomach contents entering the chest cavity or chronic acid reflux.

.avif)
This vital procedure creates a direct opening into the stomach through the abdominal wall, allowing for the placement of a feeding tube when normal eating is impossible or insufficient to maintain adequate nutrition.
What happens during surgery?
Using either an open surgical approach or minimally invasive techniques when appropriate, your surgeon makes an incision in the upper abdomen to access the stomach. A small opening is created in the stomach wall, and a specialized feeding tube is inserted and secured in place. The tube is then brought through the abdominal wall, creating a stable pathway for nutrition delivery. The entire procedure typically takes 30-60 minutes under general anesthesia.
Benefits:
Reliable route for nutrition, hydration, and medication delivery
Bypasses swallowing difficulties caused by neurological conditions or head and neck disorders
More comfortable and discreet than long-term nasogastric tubes
Reduces risk of aspiration pneumonia in patients with swallowing dysfunction
Easily maintained and managed once healing is complete
Potential for removal if normal eating ability returns
Open gastrostomy provides essential nutritional support for patients unable to eat adequately by mouth, ensuring proper nutrition and medication delivery while improving comfort and quality of life for those with long-term feeding challenges.
This targeted procedure creates a direct opening into the jejunum (middle section of the small intestine) through the abdominal wall, allowing for feeding tube placement when stomach access is contraindicated or bypassed.
What happens during surgery?
Using either an open or minimally invasive approach based on your specific needs, your surgeon makes an incision in the abdomen to access the jejunum portion of the small intestine. A small opening is created in the intestinal wall, and a specialized feeding tube is inserted and secured in place. The tube is then brought through the abdominal wall, establishing a stable pathway for nutrition delivery beyond the stomach. The entire procedure typically takes 45-90 minutes under general anesthesia.
Benefits:
Provides crucial nutritional support when stomach feeding isn't possible
Bypasses the stomach entirely for patients with gastric outlet obstruction or after gastric surgery
Reduces risk of aspiration in patients with severe gastroesophageal reflux
Allows for specialized formula delivery directly to the small intestine
Can be temporary or permanent depending on the patient's needs
Preserves nutritional status during treatment of complex gastrointestinal conditions
Jejunostomy offers essential nutritional support for patients with upper digestive tract disorders, ensuring proper delivery of nutrients to the small intestine while avoiding the stomach when necessary due to disease, obstruction, or previous surgical intervention.

.svg)

All our stomach procedures are performed by our highly trained surgical team using state-of-the-art equipment and techniques. We're committed to providing you with the most effective, specialized care for gastric conditions because we believe you deserve:
Relief from chronic stomach pain and digestive discomfort
Expert treatment of conditions like ulcers, tumors, and reflux disease
Minimally invasive approaches when appropriate for faster healing
Preservation of stomach function and digestive capabilities
Improved nutritional absorption and overall digestive health
Reduced dependency on long-term medication regimens
Comprehensive care from diagnosis through recovery and beyond
Dr. Richard Nguyen is a board-certified General Surgeon with over 20 years of surgical expertise and fellowship training in Minimally Invasive and Bariatric Surgery from Vanderbilt University. Since establishing his San Jose surgical practice in 2007, he has pioneered innovative surgical techniques, including single-incision laparoscopic procedures and mastery of the da Vinci Robotic Surgical System. Beyond his acclaimed bariatric surgery practice, he has earned national recognition for his specialized expertise in both non-mesh and advanced mesh hernia repairs, sports hernia surgery, and serves as a critical approach surgeon for anterior spine access procedures. Dr. Nguyen combines technical surgical precision with personalized patient care across multiple premier facilities throughout the South Bay Area, including San Jose, Los Gatos, and surrounding communities.
I would refer Doctor Nguyen to anyone, in fact I have and they have all had the same experience as me. He is truly great. I owe all my success to Doctor Nguyen and I thank him for all the work he has done for me and continues to do so. He is extremely amazing, and I am very grateful to him.
At 50, I now have a life I had only dreamed of a year before. My body tells me if I am done eating. This surgery is a tool that I have used to the fullest. It is not an easy way out. It still took work. But I honestly know that I would not be living this amazing new life if I didn’t step forward to embrace this life-saving surgery.
Dr. Nguyen has changed my life completely. I feel so much better and I also feel like I’ve got control of my life again…I had high blood pressure, diabetes and cholesterol. I took at least 5 different medications for the past 30 years. NOW, after surgery I take no medications only vitamins!
Wondering which surgical procedure might be right for your condition? We're here to help you understand your treatment options and develop a personalized surgical plan. Contact our office today to schedule a consultation.
Your path to improved health may be more achievable than you think—with advanced surgical techniques leading to faster recovery, reduced complications, and a significantly enhanced quality of life.