You've tried every medication your doctor prescribed, followed strict dietary guidelines, eliminated trigger foods, and taken acid blockers religiously – yet your ulcer continues to cause pain, discomfort, and disruption to your daily life. When peptic ulcers become resistant to medical treatment or develop serious complications, surgical intervention may be the key to finally achieving lasting relief and preventing life-threatening problems.
Dr. Nguyen at Lifetime Surgical has extensive experience treating complex peptic ulcer disease using the most advanced minimally invasive surgical techniques available. His expertise in both emergency and elective ulcer surgery ensures that patients receive optimal care whether they're facing urgent complications or seeking definitive treatment for chronic, treatment-resistant ulcers.
Understanding when ulcers require surgical treatment, what modern surgical options are available, and how to prevent future problems can help patients make informed decisions about their care. While most ulcers respond well to medical treatment, those that don't may benefit significantly from appropriate surgical intervention.
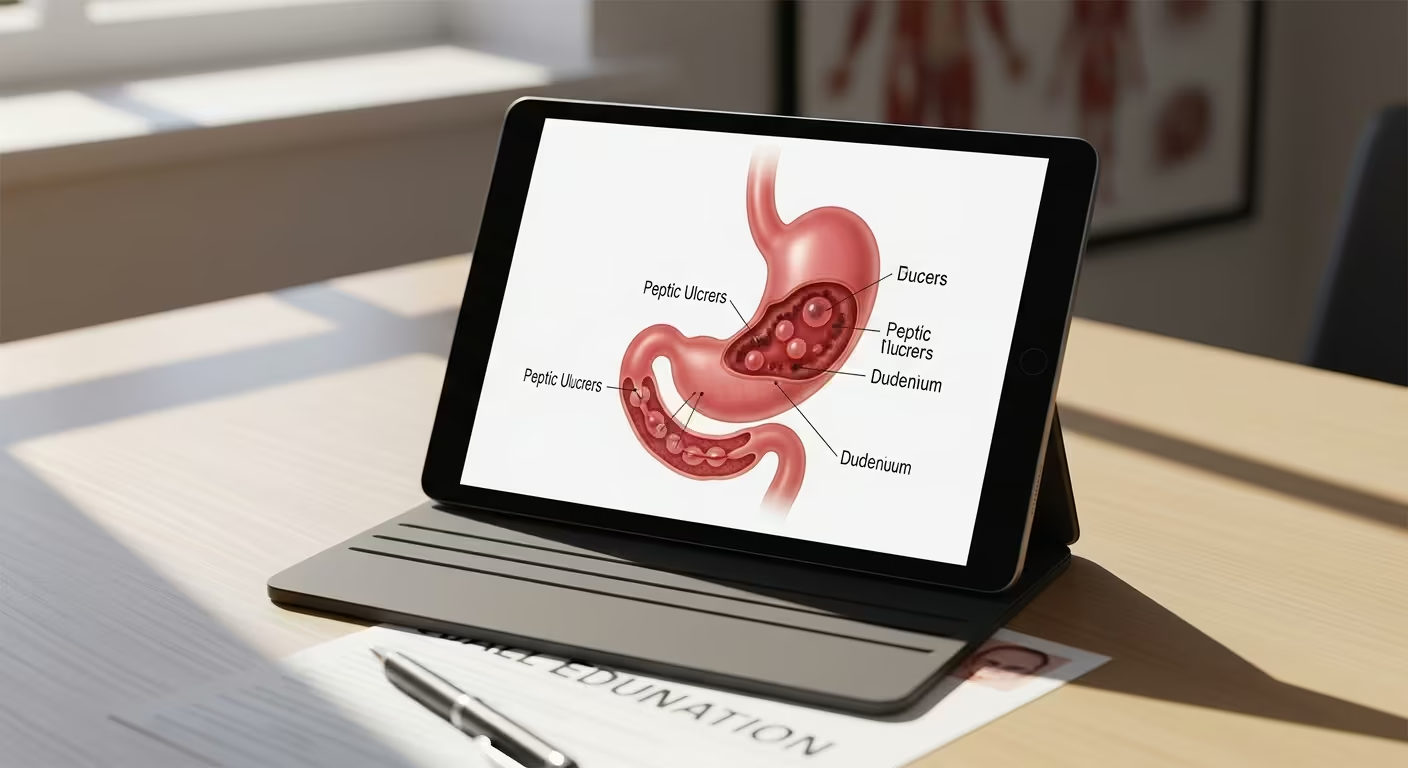
Peptic ulcers are open sores that develop in the lining of the stomach (gastric ulcers) or the upper portion of the small intestine (duodenal ulcers). While most ulcers heal with appropriate medical treatment, some become complicated, causing serious symptoms and potentially life-threatening problems that require surgical intervention.
The primary causes of peptic ulcers include infection with Helicobacter pylori bacteria, long-term use of nonsteroidal anti-inflammatory drugs (NSAIDs), and excessive stomach acid production. In most cases, treating the underlying cause – whether through antibiotics for H. pylori or stopping problematic medications – allows ulcers to heal completely.
However, some ulcers become complicated either because they don't respond to appropriate medical treatment, because they're associated with underlying conditions that prevent healing, or because they develop acute complications that require immediate surgical attention. Understanding these complications helps patients recognize when surgery becomes necessary.
The location and characteristics of an ulcer influence both its symptoms and the likelihood that it will require surgical treatment. Duodenal ulcers and gastric ulcers have different patterns of complications and may require different surgical approaches when conservative treatment fails.
Refractory ulcers are those that fail to heal despite adequate medical treatment, including appropriate acid suppression therapy and treatment of H. pylori infection when present. These ulcers typically persist or recur after 8-12 weeks of optimal medical therapy.
Incomplete H. pylori eradication is one of the most common causes of ulcer treatment failure. Some strains of H. pylori bacteria are resistant to standard antibiotic regimens, requiring alternative treatment approaches or surgical intervention when medical treatment repeatedly fails.
Continued NSAID use either intentionally or inadvertently can prevent ulcer healing. Some patients require NSAIDs for other medical conditions and cannot discontinue them, making ulcer healing difficult or impossible with medical therapy alone.
Zollinger-Ellison syndrome and other conditions causing excessive acid production can lead to ulcers that are resistant to standard acid suppression therapy. These conditions may require surgical treatment of both the underlying condition and the resulting ulcers.
Giant ulcers larger than 2-3 centimeters in diameter are more likely to be refractory to medical treatment and may require surgical intervention for healing, especially if they're associated with significant scarring or distortion of normal anatomy.
Certain ulcer complications represent surgical emergencies that require immediate intervention to prevent life-threatening consequences. These complications can develop suddenly, even in patients who were previously managing their ulcers with medical treatment.
Perforation occurs when an ulcer erodes completely through the stomach or duodenal wall, creating a hole that allows stomach contents to spill into the abdominal cavity. This complication causes severe abdominal pain and can lead to life-threatening infection if not treated immediately.
Massive bleeding from ulcers can cause significant blood loss requiring emergency surgery to control the bleeding source. While many bleeding ulcers can be treated with endoscopic procedures, some require surgical intervention for definitive control.
Gastric outlet obstruction develops when ulcers cause swelling or scarring that blocks the passage of food from the stomach into the small intestine. This complication typically develops gradually but can become severe enough to require emergency surgery.
Penetration occurs when an ulcer erodes through the stomach or duodenal wall into adjacent organs like the pancreas or liver. This complication often causes severe, constant pain that doesn't respond to typical ulcer medications.
Advanced age increases the risk of ulcer complications, as older patients may have reduced healing capacity and are more likely to be taking medications that interfere with ulcer healing.
Multiple medical conditions can impair healing and increase complication risk. Conditions like diabetes, kidney disease, and autoimmune disorders can affect the body's ability to heal ulcers effectively.
Smoking significantly impairs ulcer healing and increases the risk of complications. The chemicals in tobacco smoke reduce blood flow to the stomach lining and interfere with the healing process.
Alcohol use can worsen ulcer symptoms and delay healing by increasing stomach acid production and directly irritating the ulcer site.
Stress from major illness, surgery, or trauma can contribute to ulcer development and may impair healing of existing ulcers.
Surgical treatment for peptic ulcers has evolved significantly over the past several decades, with modern approaches focusing on minimally invasive techniques that address the underlying problem while preserving as much normal anatomy and function as possible.
Laparoscopic repair has become the preferred approach for many ulcer surgeries, offering the benefits of smaller incisions, faster recovery, and reduced complications compared to traditional open surgery. This approach can be used for both emergency and elective ulcer procedures.
Robotic-assisted surgery provides enhanced precision and visualization for complex ulcer repairs, particularly when dealing with difficult anatomy or previous surgical scarring. The enhanced dexterity of robotic instruments can be valuable in challenging cases.
Single-incision techniques may be appropriate for select cases, further reducing the invasiveness of ulcer surgery while maintaining effectiveness. This approach requires specialized expertise but can provide excellent cosmetic outcomes.
Simple closure with omental patch is the most common procedure for perforated ulcers, involving closing the hole in the stomach or duodenum and covering it with a piece of omentum (fatty tissue from the abdomen) to reinforce the repair.
Pyloroplasty involves widening the outlet from the stomach to improve gastric emptying and reduce acid production. This procedure can be particularly effective for ulcers associated with gastric outlet obstruction or delayed gastric emptying.
Vagotomy involves cutting the vagus nerves that stimulate acid production in the stomach. While less commonly performed today due to effective acid-suppressing medications, this procedure may still be appropriate for selected cases of refractory ulcers.
Antrectomy involves removing the lower portion of the stomach (antrum) where much of the stomach's acid-producing cells are located. This procedure is typically reserved for complicated cases where other approaches haven't been successful.
Highly selective vagotomy involves cutting only specific branches of the vagus nerve while preserving those that control stomach emptying. This approach reduces acid production while maintaining normal gastric function.
Emergency surgery for ulcer complications focuses primarily on controlling life-threatening problems like bleeding or perforation. The immediate goal is patient stabilization, with definitive ulcer treatment often addressed in a staged approach.
Elective surgery allows for more comprehensive evaluation and planning, potentially permitting more sophisticated procedures that address both the ulcer and underlying contributing factors. This approach often provides better long-term outcomes when surgery can be planned in advance.
Damage control surgery may be necessary in critically ill patients with perforated ulcers, involving temporary measures to control contamination and bleeding with plans for definitive repair once the patient is stabilized.
Ulcer location influences the choice of surgical approach, as duodenal ulcers and gastric ulcers may require different procedures based on their anatomical considerations and blood supply patterns.
Patient age and health status affect surgical risk and recovery potential, influencing the choice between more conservative repairs and more extensive procedures that might provide better long-term outcomes.
Previous surgical history can complicate ulcer surgery due to adhesions and altered anatomy, potentially requiring more complex procedures or open surgical approaches.
Underlying medical conditions such as Zollinger-Ellison syndrome may require surgical treatment of the underlying condition in addition to ulcer repair for optimal outcomes.
Recovery from ulcer surgery involves both immediate post-operative healing and long-term lifestyle adjustments to promote ulcer healing and prevent recurrence. Understanding what to expect helps patients prepare for the recovery process and optimize their outcomes.
Hospital stay typically ranges from 2-7 days depending on the complexity of the surgery and whether it was performed emergently or electively. Minimally invasive procedures generally allow for shorter hospital stays.
Pain management requires a balanced approach that controls discomfort while allowing for early mobilization and return of normal digestive function. Modern pain management techniques minimize the need for medications that might interfere with healing.
Nasogastric decompression may be necessary initially to allow the stomach to rest and the surgical repair to heal. This involves a temporary tube through the nose to drain stomach contents.
Gradual diet progression begins with clear liquids and advances slowly to regular foods as the digestive tract heals and normal function returns. This progression is typically more gradual than after other types of surgery.
Monitoring for complications includes watching for signs of leakage from surgical repairs, bleeding, infection, or other problems that can occur after ulcer surgery.
Bland diet emphasis during the first few weeks after surgery helps minimize irritation to healing tissues. Foods that are easy to digest and don't stimulate excessive acid production are preferred initially.
Small, frequent meals are easier to digest and help prevent excessive stretching of the stomach during healing. Large meals can cause discomfort and may interfere with healing.
Avoiding irritating substances including alcohol, caffeine, spicy foods, and acidic foods helps promote healing and reduces the risk of complications during recovery.
Adequate protein intake is crucial for healing, as protein provides the building blocks needed for tissue repair and recovery from surgery.
Hydration maintenance is important for healing, though patients may need to be careful about fluid timing to avoid excessive stomach fullness during meals.
Continued acid reduction through dietary choices helps prevent ulcer recurrence. This includes avoiding foods that stimulate acid production and eating patterns that minimize acid exposure to healing tissues.
Regular meal timing helps regulate stomach acid production and prevents periods of excessive acid exposure that might contribute to ulcer recurrence.
Portion size management may be necessary long-term, particularly after procedures that alter stomach anatomy or function. Some patients find that smaller, more frequent meals remain preferable indefinitely.
Individual food tolerance varies among patients, and many find they need to permanently avoid certain foods that cause discomfort or symptoms. Common problematic foods include spicy foods, citrus, tomatoes, and caffeine.
Vitamin B12 absorption may be affected by some ulcer surgeries, particularly those involving vagotomy or gastric resection. Regular monitoring and supplementation may be necessary.
Iron absorption can be impaired after certain types of ulcer surgery, potentially leading to anemia if not monitored and treated appropriately.
Overall nutritional status should be monitored regularly, particularly in patients who have undergone more extensive procedures or who have difficulty maintaining adequate oral intake.
While surgery can effectively treat complicated ulcers, preventing recurrence requires ongoing attention to the underlying factors that contribute to ulcer development. Understanding and addressing these factors is crucial for long-term success.
Eradication confirmation after antibiotic treatment is essential, as incomplete eradication is a major cause of ulcer recurrence. Follow-up testing should be performed to ensure that the infection has been completely eliminated.
Alternative treatment regimens may be necessary for patients with antibiotic-resistant H. pylori strains. These may involve different antibiotic combinations or longer treatment courses.
Regular surveillance may be appropriate for patients with a history of H. pylori infection, particularly those who have had complicated ulcers or multiple episodes of infection.
NSAID alternatives should be explored for patients who require anti-inflammatory treatment. Alternative medications or topical preparations may provide relief without the gastrointestinal risks of oral NSAIDs.
Gastroprotective agents may be necessary for patients who must continue taking NSAIDs or other ulcerogenic medications. Proton pump inhibitors or other protective medications can help reduce ulcer risk.
Medication review should be performed regularly to identify any new medications that might increase ulcer risk and to ensure that protective medications are being used appropriately.
Smoking cessation is crucial for preventing ulcer recurrence, as smoking significantly increases the risk of ulcer development and impairs healing. Comprehensive smoking cessation programs can help patients successfully quit.
Alcohol moderation helps reduce stomach irritation and acid production that can contribute to ulcer recurrence. Complete abstinence may be necessary for some patients with severe ulcer disease.
Stress management techniques can help reduce the physiological factors that contribute to ulcer development. Stress reduction strategies, exercise, and relaxation techniques may be beneficial.
Regular meal patterns help regulate stomach acid production and reduce periods of excessive acid exposure that might contribute to ulcer recurrence.
Regular medical monitoring helps identify early signs of ulcer recurrence and allows for prompt treatment before complications develop. This typically involves periodic symptom assessment and sometimes endoscopic surveillance.
Symptom awareness education helps patients recognize early signs of ulcer recurrence so they can seek treatment promptly. Early intervention can often prevent the development of complications.
Emergency action plans ensure that patients know how to respond if they develop signs of serious ulcer complications like bleeding or perforation. Having clear instructions can be life-saving in emergency situations.
Most patients who undergo surgical treatment for complicated peptic ulcers experience excellent long-term outcomes with significant improvement in their quality of life. Understanding what to expect helps set realistic expectations for recovery and long-term management.
Pain relief is typically excellent after successful ulcer surgery, with most patients experiencing complete or near-complete resolution of their ulcer-related pain. Some patients are amazed at how much better they feel once their ulcer is properly treated.
Digestive function usually returns to normal or near-normal after recovery from ulcer surgery, though some patients may need to make permanent dietary adjustments based on the specific procedure performed.
Activity restoration allows most patients to return to all their previous activities without restrictions related to their ulcer disease. The freedom from constant pain and dietary restrictions can be life-changing.
Eating patterns may require some long-term modifications, but most patients can enjoy a varied diet without the severe restrictions they may have needed before surgery.
Work and social activities can typically be resumed fully once recovery is complete. Many patients find they can participate in activities they had avoided due to ulcer symptoms.
Exercise tolerance usually improves significantly after successful ulcer treatment, as patients no longer have to avoid activities that might trigger ulcer pain.
Low recurrence rates are achieved when underlying causes are properly addressed and preventive measures are followed. Modern surgical techniques combined with appropriate medical management provide excellent long-term results.
Risk factor modification significantly reduces the likelihood of ulcer recurrence. Patients who successfully eliminate H. pylori infection, stop smoking, and manage their medications appropriately have very low recurrence rates.
Early detection of any recurrence allows for prompt treatment that can usually prevent the development of complications requiring additional surgery.
The success of ulcer surgery depends significantly on surgeon experience and expertise, particularly for complex cases or emergency situations. Dr. Nguyen's extensive experience with both emergency and elective ulcer surgery ensures optimal outcomes for patients facing these challenging conditions.
Surgical expertise in ulcer surgery requires understanding of both the acute management of ulcer complications and the long-term factors that contribute to ulcer recurrence. Experience with minimally invasive techniques allows for optimal outcomes with faster recovery when possible.
Emergency surgical capability is crucial for ulcer complications, as these conditions often require immediate intervention. Having access to experienced surgical teams 24 hours a day can be life-saving when ulcer complications develop.
Dr. Nguyen's comprehensive approach to ulcer surgery includes not only expert surgical technique but also attention to the underlying factors that contribute to ulcer development and recurrence. This comprehensive care helps ensure the best possible long-term outcomes.
Multidisciplinary care coordination involving gastroenterologists, nutritionists, and other specialists ensures that all aspects of ulcer disease are addressed comprehensively, from acute treatment through long-term prevention.
For patients who have struggled with chronic, treatment-resistant ulcers, surgical intervention can provide the definitive solution they've been seeking. Modern surgical techniques offer excellent outcomes with minimal disruption to normal life once recovery is complete.
The goal of ulcer surgery is not just to treat the immediate problem but to provide long-term freedom from ulcer disease through comprehensive treatment that addresses underlying causes and prevents recurrence.
Dr. Nguyen's expertise in ulcer surgery, combined with a comprehensive approach to prevention and follow-up care, helps ensure that patients achieve lasting relief from their ulcer disease.
Recovery from ulcer surgery typically results in significant improvement in quality of life, allowing patients to return to activities and foods they may have avoided for months or years due to ulcer symptoms.
If you're struggling with ulcers that won't heal despite medical treatment, or if you've experienced ulcer complications, don't continue to suffer in silence. Dr. Nguyen at Lifetime Surgical has extensive experience with both emergency and elective ulcer surgery using the most advanced minimally invasive techniques available. His comprehensive approach addresses both immediate treatment needs and long-term prevention strategies. Contact our Los Gatos office today to schedule a consultation and explore how modern surgical solutions can provide the lasting relief you've been seeking from chronic ulcer disease.
Wondering which surgical procedure might be right for your condition? We're here to help you understand your treatment options and develop a personalized surgical plan. Contact our office today to schedule a consultation.
Your path to improved health may be more achievable than you think—with advanced surgical techniques leading to faster recovery, reduced complications, and a significantly enhanced quality of life.